26
2024
-
12
Esthetic Outcome of Immediate Implant Placement Using Customized Healing Abutment in Anterior Region.
Esthetic Outcome of Immediate Implant Placement Using Customized Healing Abutment in Anterior Region.
Esthetic Outcome of Immediate Implant Placement Using Customized Healing Abutment in Anterior Region.
ABSTRACT
Statement of problem: Providing a definitive anterior implant placement restoration with proper esthetic and peri-implant soft tissue contour is important for immediate implant placement and achieving a good immediate implant esthetic outcome.
Material and method: immediate implant placement to replace non restorable teeth in the maxillary anterior region. The dentist extracted the tooth and immediately inserted an implant. They fabricated customized healing abutments using a Cervico mold and connected them to the dental implant. After 3 months, they performed intraoral scanning to fabricate a definitive crown.
Conclusion: Easy clinical technique to create proper emergence profile through customized healing abutment using the Cervico device. The use of Cervico device for the construction of customized healing abutments prepares soft tissue for the prosthetic stage preserving its contours and eliminating the need for reopening surgery for immediate as well as for early implant placement.
Keywords: Customized healing abutment, emergence profile, immediate placement, soft tissue management
INTRODUCTION
Esthetics is of the most importance while rehabilitating maxillary anterior region with dental implants. Several variables influence the anterior esthetics, including the patient’s smile line, the location of the dental implant, the periodontium biotype, the tooth form, the position of neighboring teeth, the bone structure at the implant site, and the timing of implant placement. Additional di culties arise during implant implantation because of the great visibility and patient expectations. The accelerated bone remodeling especially in the maxillary anterior region makes the preservation of the peri-implant tissue and contour crucial 1 , 2. After extracting the tooth, the clinician immediately placed an implant using various clinical approaches to minimize bone loss and enhance implant success, favoring less invasive procedures. Minimally invasive tooth extraction, avoiding unnecessary flap release, minimizes tissue disruption, and conserves alveolar bone.3, 4, 5 Regardless of implant placement timing and according to the clinical situation, provisional restoration is crucial. It can provide immediate aesthetics and function while the implant integrates as it preserves soft tissue contours simplifying subsequent treatment stages6, 7. Once secondary stability is achieved, indicating complete integration, the final prosthesis can be manufactured, benefiting from preserved soft tissue contours for more predictable results. Adequate primary stability, exceeding 35 N cm or an implant stability quotient above 70, is crucial for the desired outcome8. Implementing comprehensive and less invasive approaches addresses post-tooth extraction bone loss, enhancing implant success for optimal aesthetic and functional outcomes. Customized healing abutments, offer a promising solution. They protect and preserve alveolar contours, eliminate the need for a second reopening surgery and provisional restorations, and expedite the soft tissue conditioning phase for natural-like restorations. This approach provides a simplified chairside technique for customizing healing abutments. It is particularly useful for immediate implants and early implant placement in the anterior region. The aim is to maintain soft tissue contours and reduce the number of clinical steps, presenting a valuable alternative to traditional methods10. The aim of the study was to evaluate the soft tissue contour between early and immediate implant placement using customized healing abutment
Materials and method
The researchers conducted this study as a prospective, double-blinded, balanced, randomized controlled clinical trial with a parallel-group design. The ethical committee of the Faculty of Dentistry at Beirut Arab University approved it under number IRB2023-H0113D-P-0494. They placed twenty-four dental implants in twelve participants indicated for bilateral immediate and early implant placement in the esthetic zone of the maxillary dental arch. The team selected these participants from individuals attending the Department of Prosthodontics at Beirut Arab University, Lebanon. Researchers explained clinical procedures and possible complications to the participants, who then signed informed consent, in line with the 1975 Declaration of Helsinki, revised in 2013.
The inclusion criteria required patients aged 20 to 40 with unrestorable bilateral teeth, a harmonious gingival contour, a thick gingival phenotype, at least 4 mm of bone apical to the root apex, a 2 mm labial plate of bone at the unrestorable tooth to be extracted, and no periapical radiolucency (Fig 1). Researchers excluded any patient suffering from medical disorders that interfere with osseointegration or soft tissue healing, active oral infections or periodontal disease, dehiscence or fenestration defects related to the tooth, poor oral hygiene, and heavy smoking habits.
They made a bench scan (Medit T-710 Tabletop Scanner) of the cast and a preoperative CBCT (3D Accuitomo 170) for each participant to construct a CAD CAM surgical guide. The implant plan aimed to engage the palatal wall, avoid pressure on the labial plate of the bone, and sit 1 mm apical to the crest. The team designed and printed a fully guided, tooth-supported surgical guide in clear acrylic resin (Dental SG Resin; Formlabs) using a 3D printer (Form2; Formlabs).(fig 2)
Figure1: Preoperative photo and panoramic view of CBCT for the patient before treatment
Figure2: Virtual design of implant placement
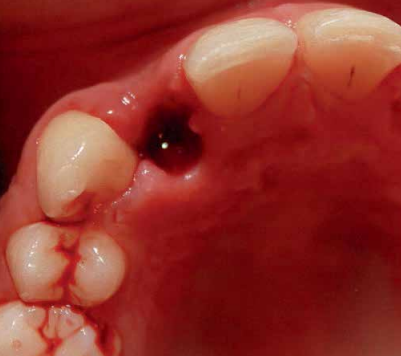
A systemic antibiotic (2g amoxicillin-clavulanic acid, per-orally) was administered to the patients 1 hour prior to the procedure. The patient’s mouth was rinsed with a solution of chlorhexidinedigluconate 0.2% for 2 minutes. After surgical guide printing, the tooth was extracted and the implant placed (IDI implant Implants Di usion International 23/25) following implant placement protocol using a fully guided CAD CAM surgical guide. 14 (fig 3,4,5)
Figure3: Extraction of upper 12 anterior teeth.
Figure4: surgical implant placement using CAD/ CAM surgical guide.
Figure5: Fully guided implant placement through the surgical guide using spoons. The implant was inserted at the planned position.
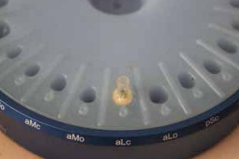
Directly after immediate implant placement, a customized healing abutment was fabricated using Cervico kit. The selection was made intraorally using a special handle to place the indicator over the restorable area. (fig 6) Utilize the anatomical shape tab from the same group as per the anterior tooth missing. The anterior suitable stock healing abutment was directly screwed on the implant analog and was fixed at the corresponding well of the silicone mold, and the custom healing abutment was fabricated with nano hybrid flowable resin (3M™ Filtek™ Supreme Flowable Composite) (Fig 7,8). Minor selective grinding, finishing, and polishing were made when necessary to achieve a smooth, lustrous tissue contact surface, and screwed to the implant. 15 (Fig 9)
Figure6: Cervico mold used for fabrication of customized healing abutment
Figure7: Custom made healing abutment for implant placement using indicator and mold of Cervico tool.
Figure8: Customized healing abutment in position.
Figure9: The provisional crown was placed.
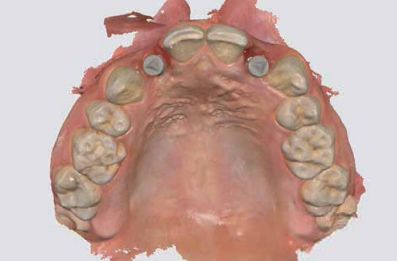
The prosthetic procedures for definitive restorations were performed 3 months after implant placement. The healing abutment was removed (Fig 10) scan body was placed in position and a digital implant level impression was made using an intraoral scanner (Medit I 700 3D scanners) (16) (Fig 11,12)
Figure10: Soft tissue healing after removal of custom-made provisional crowns.
Figure11: Scan body connected to the implant for intraoral scanning.
The clinician used Exocad to design the restoration (fig. 13) and milled it from a super translucent multilayered zirconia (KATANA Zirconia STML; Kuraray Noritake). They cemented the milled restoration onto the Ti-base with resin cement (RelyX Unicem; 3M ESPE). Next, they connected the definitive restoration to the implant and tightened the Ti-base screw to 20 Ncm, following the manufacturer’s instructions. They sealed the screw access channel with sterilized PTFE and photopolymerized composite resin (Filtek Supreme Ultra; 3M ESPE). The clinician then evaluated the definitive restoration for centric and eccentric occlusal contacts before finishing and polishing it (fig 14,15).
Figure12: Virtual view of scan body after scanning.
Figure13: Virtual crown designed using exocad software.
Figure14: Zirconium crown cemented to Ti-base abutment.
Figure15: Final definitive crowns after screwing intraorally for di erent cases.
Discussion
The anterior region of the maxilla is frequently termed the aesthetic zone due to its high visibility and influence on facial appearance. Single tooth implant replacement in this region can present many clinical challenges. Not only must the crown conform in contour, shade, and texture to its neighbors, but the gingiva must also be in symmetry and harmony with the adjacent tissues. As we have learned, once a maxillary anterior tooth is extracted, the collapse of the socket wall begins in a buccal to palatal direction. This is accentuated even more in a socket with a thin or non existent buccal plate. In addition, the crestal height of the extraction socket begins to move apically.
This can leave a large concavity in the buccal gingival tissue, resulting in a prosthesis that will not be symmetrical to the adjacent dentition. Meticulous planning is necessary for implant placement in the esthetic zone. Numerous treatment modalities have been developed for the long-term temporization and previsualization of anterior implant cases.
Case reports are appearing in the literature of immediate implant placement and immediate temporization with acrylic crowns. It is important to stress that immediate implant placement does not prevent the remodeling or resorptive processes associated with a tooth’s loss. Thorough diagnostic assessments, including radiographic imaging and clinical evaluations, are crucial for understanding the patient›s unique anatomy, bone quality, and the condition of the extraction site. Clearly defined treatment objectives should align with the patients esthetic and functional expectations. This includes determining the ideal implant position and emergence profile. Early implant placement, which refers to implant placement following complete soft tissue coverage of the extraction socket, was introduced as a viable treatment alternative. It has been suggested that the soft tissue healing allows for the resolution of local pathology and provides enhanced soft tissue volume.
Several studies have shown promising clinical outcomes for implants placed according to the early placement protocol. However, it is necessary to compare the clinical outcomes of implants placed according to the early implant placement protocol with those of implants placed according to the immediate or the delayed implant placement protocols. In this study, the split mouth technique with immediate implant and early implant in the anterior region is used for various reasons. Firstly, it improved the implant›s primary stability by avoiding buccal wall engagement, reducing the need for jumping distance, and minimizing the risk of implant failure. The use of moderate insertion torque (32-50 Ncm) may reduce the risk of implant failure (HEBA 2020).
Using Cone-Beam Computed Tomography (CBCT) with immediate and early implant placement in the anterior region is crucial because it improves diagnostic accuracy. The CBCT provides accurate three dimensional images that help in proper diagnosis and treatment planning, especially in the anterior maxilla where the risk of damaging the buccal plate during extraction is higher. Also, reduced resorption and healing time: Immediate implant placement with CBCT reduces alveolar bone resorption after extraction, leading to better function and aesthetics. It also eliminates the need for a waiting period of 10-12 months for socket healing, reducing the overall treatment time and psychological stress on the patient. It enhanced predictability and eciency where research showed with Mikic et al. (2022)22 that using CBCT for bone density assessment is significantly correlated with implant stability, improving predictability and eciency of implant planning and placement. This technology allows for better control over implant placement, ensuring optimal outcomes.
Utilizing digital technologies for treatment planning enhances precision. Computer-aided design (CAD) and computer-aided manufacturing (CAM) systems contribute to accurate implant placement and customized abutment design. Our study introduced intra-oral scanning and digital data measurement as new methods for assessing the dimensional changes of soft
tissue during the healing period in one-step recording direct from the source and ensured this measurement protocol is more accurate than the conventional step which cumulates routine error in the impression taking with weight material, the poured stone model and hand-manual measuring. The use of CAD/CAM technology in implant crown design has the potential to improve the accuracy and eciency of the restoration process, providing patients with a functional and aesthetic solution to their dental needs24. Healthy peri-implant gingiva is important to ensure a good emergence profile, particularly in the esthetic zone.
It plays a role in preventing periimplant disease by forming a barrier to eciently protect underlying bone and prevent access to microorganisms. In addition, after the final restoration, time may be required for soft tissue to fill the embrasure, which is more predictable with healthy tissue, shows adequate interdental papilla, well contoured gingiva, and the presence of stippling and no inflammation, indicative of healthy peri-implant tissue25 The use of provisional abutments and immediate temporization have a proven track record of their ability to produce optimal esthetics and to guide the tissue response during the healing phase.
Customization of the healing abutment had more dimensional improvement in soft tissue healing when compared with stock healing abutment. First, because of flapless protocol, a stock healing abutment is unable to completely seal the underlying alveolar socket in the immediate implantation. If this abutment can’t be avoided, using a flap elevation procedure is needed to seal the grafting material.26.
Conclusion
The use of customized healing abutments seemed to be an appropriate solution to support and maintain the soft and hard tissue contours after immediate implant placement in both the anterior regions. This reinforces the importance of long-term monitoring and care in the management of dental implants, emphasizing that immediate placement strategy can achieve comparable outcomes in terms of bone health and implant stability using customized healing abutment, provided that appropriate post operative care and follow up protocols.
References :
1- Hämmerle CF, Tarnow D. The etiology of hard- and softtissue deficiencies at dental implants: Anarrative review. J Clin Periodontol.2018; 45 :S267 – S277.
2- Altay A, Sindel A, Hüseyin H, Nelli OM. Esthetic evaluation of implant-supported single crowns: a comparison of objective and patient reported outcomes. Int J Implnt Dent. 2019; 5(1):2- 4
3- Barone A, Rispoli L, Vozza I, Quaranta A, Covani U. Immediate restoration of single implants placed immediately after tooth extraction. Journal of periodontology. 2006 Nov;77(11):1914-20.
4- Hämmerle CH, Tarnow D. The etiology of hard-and softtissue deficiencies at dental implants: A narrative review. Journal of clinical periodontology. 2018 Jun;45:S267-77.
5- Araujo MG, Lindhe J. Peri-implant health. Journal of periodontology. 2018 Jun;89:S249-56.
6- Baltayan S, Pi-Anfruns J, Aghaloo T, Moy PK. The predictive value of resonance frequency analysis measurements in the surgical placement and loading of endosseous implants. Journal of Oral and Maxillofacial Surgery. 2016 Jun 1;74(6): 1145- 52.
7- Passoni BB, Marques de Castro DS, de Araújo MA, de Araújo CD, Piatelli A, Benfatti CA. Influence of immediate/ delayed implant placement and implant platform on the periimplant bone formation. Clinical oral implants research. 2016 Nov;27(11):1376-83.
8- Cosyn J, De Lat L, Seyssens L, Doornewaard R, Deschepper E, Vervaeke S. The electiveness of immediate implant placement for single tooth replacement compared to delayed implant placement: A systematic review and meta-analysis. Journal of Clinical Periodontology. 2019 Jun;46:224-41.
9- Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single tooth implant crowns: the pink esthetic score. Clinical oral implants research. 2005 Dec;16(6):639-44.
10- Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, Buser D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a crosssectional, retrospective study in 45 patients with a 2-to 4-year follow-up using pink and white esthetic scores. Journal of periodontology. 2009 Jan;80(1):140-51.
11- Kuthning M, Hundt F. Aspects of vulnerable patients and informed consent in clinical trials. GMS German Medical Science. 2013;11.
12- Dawson A, Martin WC, Polido WD, editors. The SAC classification in implant dentistry. Quintessenz Verlag; 2022 Mar 30.
13- Chrcanovic BR, Martins MD, Wennerberg A. Immediate placement of implants into infected sites: a systematic review. Clinical implant dentistry and related research. 2015 Jan;17:e1-6.
14- Del Fabbro M, Bianchessi C, Del Lupo R, Landi L, Taschieri S, Corbella S. Platform switching vs standard implants in partially edentulous patients using the Dental Tech Implant System: clinical and radiological results from a prospective multicenter study. Clinical oral investigations. 2015 Dec;19:2233-44. 15- Schirdewan I. ConsEuro Conference 2019, Berlin, June 14-
15. Clinical Oral Investigations. 2019 May 1; 23(5): 2515-72.
16- Lee B, Nam NE, Shin SH, Lim JH, Shim JS, Kim JE. Evaluation of the trueness of digital implant impressions according to the implant scan body orientation and scanning method. Applied Sciences. 2021 Mar 29;11(7): 3027.
17- Sailer I, Barbato L, Mojon P, Pagliaro U, Serni L, Karasan D, Cairo F. Single and partial tooth replacement with fixed dental prostheses supported by dental implants: A systematic review of outcomes and outcome measures used in clinical trials in the last 10 years. Clinical oral implants research. 2023 May;34:22-37.
18- Soegiantho P, Suryawinata PG, Tran W, Kujan O, Koyi B, Khzam N, Algarves Miranda L. Survival of single immediate implants and reasons for loss: a systematic review. Prosthesis. 2023 Apr 17; 5(2): 378-424.
19- Bassir SH, El Kholy K, Chen CY, Lee KH, Intini G. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. Journal of periodontology. 2019 May;90(5):493-506.
20- Heba MB. stability and marginal bone loss of early loaded slactive implant with flapped and flapless approaches. International Journal of Medical Dentistry. 2020 Jan 1;24(1).
21- Weiss R, Read-Fuller A. Cone beam computed tomography in oral and maxillofacial surgery: an evidence-based review. Dentistry journal. 2019 May 2;7(2) :52.
22- Mikic M, Vlahovic Z, Stevanović M, Arsic Z, Mladenovic R. The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study. Tomography. 2022 May 11; 8(3): 1293 -306.
23- Barros I, Carvalho GG, Leão MO, Kassis EN. Major approaches to laser therapy in regenerative processes in bucco-maxillofacial bone defects: a concise systematic review. MedNEXT Journal of Medical and Health Sciences. 2023 Aug 4;4(3).
24- Mühlemann S, Hjerppe J, Hämmerle CH, Thoma DS. Production time, electiveness and costs of additive and subtractive computer-aided manufacturing (CAM) of implant prostheses A systematic review. Clinical Oral Implants Research. 2021 Oct;32:289-302.
25- Nayak DG, Uppoor A, Abhay K, editors. Fundamentals of Periodontology and Oral Implantology-EBook. Elsevier Health Sciences; 2021 Sep 4.
26- de Araújo Nobre M, Antunes C, Lopes A, Ferro A, Nunes M, Gouveia M, Azevedo Coutinho F, Salvado F. Partial Implant Rehabilitations in the Posterior Regions of the Jaws Supported by Short Dental Implants (7.0 mm): A 7-Year Clinical and 5-Year Radiographical Prospective Study. Journal of Clinical Medicine. 2024 Mar 8; 13(6): 1549
Authors:
-Sara N. El Touliani 1* , Ahmed M. Abdelhamid 2 , Yasser M.Aly 3 , Nada M. H. Fahmy 4 -Sara El Touliani, BDS, MSc, Lecturer of Prosthodontics, Faculty of Dentistry, Beirut Arab University, Beirut, Lebanon. -Ahmed M. Abdelhamid, BDS, MSc, PhD, Professor of Prosthodontics, Faculty of Dentistry, Alexandria University, Egypt. -Yasser M.Aly, BDS, MSc, PhD, Associate Professor of Prosthodontics, Faculty of Dentistry, Alexandria University, Egypt. -Nada M. H. Fahmy, BDS, MSc, PhD, Lecturer of Oral and Maxillofacial Surgery, Faculty of Dentistry, Arab Academy for Science, Technology and Maritime Transport
Correspondence:
Sara El Touliani Department of Oral Rehabilitation Sciences, Division of Prosthodontics, Faculty of Dentistry, Beirut Arab University, Riad El Solh, Beirut, P.O. Box 11-5020, Lebanon. Email: s.tliani@bau.edu.lb . Telephone: 009613884280.
ORCID:
Sara El Touliani: https://orcid.org/0009-0005- 2098-6182 -Ahmed M. Abdelhamid: https://orcid.org/0000- 0002-3200-866X -Yasser M.Aly: https://orcid.org/0000-0001-9119- 1145 -Nada M.H. Fahmy: https://orcid.org/0009-0000- 4074-4416 All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ST, NF. The first draft of the manuscript was written by ST and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. ST, NF: Conceptualization, Methodology, Software, Data curation, WritingOriginal draft preparation, Visualization, Investigation. A.A, YA: Reviewing and editing. All authors read and approved the final manuscript.
Key words:
Previous page
Previous page